I haven’t been able to post as many updates on here as I would like to because we’ve just been so busy. So I created a Facebook page where I will post small daily updates. Search for “Jaxsons Got Guts” & like the page to see what’s happening. I will still continue to write more in depth posts on here, it just won’t be as frequent. Again thank you all for following his journey and supporting us along the way!
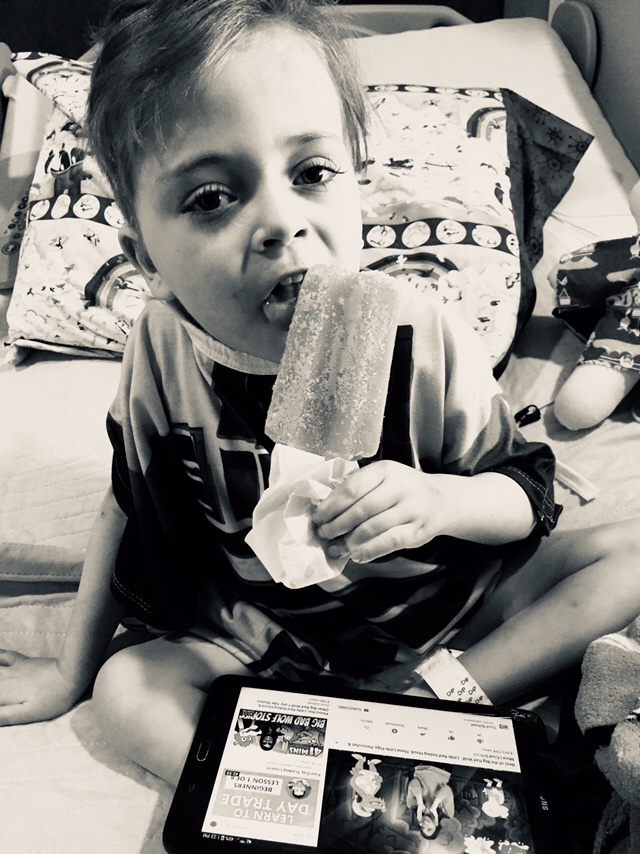
Jaxson has made some big moves since my last update. He got extubated on 4/23 and turned FIVE years old on 4/25! He still requires oxygen during the day and cpap at night while he’s sleeping- that will be his new baseline because of the way his diaphragm sits. He has been weaned off all the opiate pain meds and the last med he is still being weaned from is Ativan. He’s been allowed sips of water (and popsicles) throughout the day for the last three days and he is excited about that. He lost some muscle from being in bed for almost two months but that too has progressed nicely. He isn’t as shaky as he was when he first got extubated and he is working on standing. And finally, after 56 days in the PICU, he got moved back up to the transplant floor.




He thoroughly enjoyed his birthday. I decorated his room in paw patrol & superheroes. He opened presents all day, got out of bed and even licked some frosting. The hospital is definitely not where anyone wants to spend their birthday, but we did what we could to make it enjoyable and memorable.






My last post was about Jaxson undergoing an enterectomy (removal of the transplanted small intestine). The anatomy of that is a little complicated now, but I will try my best to explain it. For reference, Jaxson still has his stomach, his duodenum (small part of the small intestine) and his colon. He also still has the donor liver, as that was not in rejection and he needs that to survive. The liver is connected to the small intestine by the bile ducts, and because of that, Jaxson still has the donor duodenum. Usually, bile would drain into the intestine and out through the colon. The surgeons did not feel comfortable connecting the donor duodenum to Jaxson’s native duodenum, so the donor duodenum is stapled off, and the bile draining into it can’t go anywhere. They placed a duodenal tube (it looks similar to a g-tube), exiting on the right side of his stomach so bile can drain out of it. He will likely have this tube long term. A few days after surgery, they noticed his liver numbers going up and his duodenal tube not draining as much bile as it should, so he had to have a biliary drainage tube placed. This tube goes into a bile duct, and exits in the middle-left side of his belly- it drains bile directly from the liver. They noticed that the duodenal tube was kind of blocking the bile duct causing it not to drain as it should, and they could’ve messed with that a little to fix it but it was too new, they didn’t want to touch it so they placed the biliary drain. This tube is likely short term. I hope I explained that right, and I hope I explained it in a way that isn’t too confusing. Jaxson will still be able to eat/drink as he did before (though he won’t absorb much and will likely be limited just as he was before transplant.) The surgeons told us Jaxson could be placed on the transplant again in a year (or sooner depending on his recovery/health).
He has been intubated and sedated for almost a month now, and he hates it- rightfully so. He’s had some problems with agitation and confusion because of the amount of opioids and benzodiazepines he has been on. He was on dilaudid after transplant up until a couple weeks ago, then they switched to fentanyl and then morphine. He’s also on ativan, ketamine and most recently to help with confusion & agitation, zyprexa. Because he has been on these so long, they also added methadone to help with withdrawals as they try to wean everything for extubation. Since adding the zyprexa, I have noticed a change in him- he’s definitely less confused. When he opens his eyes, he is actually able to focus and when he gets agitated he’s able to calm a lot more easier/quicker. I was really happy when supportive care, who generally manages these meds, came in today and said they were going to tell the nurses to start using the opioids as a last resort (because some are quick to give them to him as soon as he moves). I also really think most of his agitation is more from the breathing tube and being restrained than actual pain, but I understand that is not a valid reason to remove it. They had plans to remove it sometime this week, but a chest x-ray taken 2 days ago looked significantly worse than the one taken the previous day so that is being held off a few more days. His sister came last week and I think that has lifted his spirits a lot. While I believe her being here will be good for his recovery, I think right now it can be a little over stimulating for him so we only have her in there for a couple hours a day. I can tell he is sooo ready to play with her and love on her again. They pushed each others buttons, but were definitely inseparable before all of this. He has a birthday in a week and i’m hoping & praying he is awake & has the breathing tube out so we can celebrate it on the exact day! I wish I had more exciting things to update on & write about, but this recovery will be a slow (but steady) one! He is one tough warrior!




Sometimes things don’t go as planned & that’s ok.
Jaxson’s body continued to reject the small intestine and so his transplant team decided it was best to remove it. I tried to prepare myself for the possibility of this outcome since about week two of rejection, so it didn’t come as a complete shock to me. Unfortunately this is not the outcome any one wanted but he was becoming more sick every day so it was the right choice. He was in surgery for 5 hours yesterday, and everything went well. The donor liver and pancreas were not rejecting (and he needs the liver to live) so they kept those in. The next few days are the most critical as he just had major abdominal surgery & has no immune system, but I’m confident he will recover well and be back to his normal happy self soon. He already looks a lot better to me and I cannot wait until he’s awake again. He’s been sedated for the last couple of weeks so I’m really excited to see his bright blue eyes, hear his sweet little voice & finally have my baby back. He will be re listed for transplant once he’s fully recovered which could be a few months or a year. So we still have a long road ahead of us, but i know he will continue to conquer anything he’s faced with.
The address for cards is:
Ronald McDonald House
Katherine dahl #1205
451 44th st
Pittsburgh,PA 15201
One month post transplant
One month post transplant and Jaxson is still actively (and severely) rejecting. They are trying what I believe is the last drug there is to try, which is called Campath. This drug in simple terms, is going to put his T cells (which help your immune system attack things) “to sleep,” because those are playing a big role in the rejection. I’m really hoping this helps because he’s been through so much, and has been on so many different drugs- he deserves a break. He will have another scope/biopsy Monday & Thursday- Monday may be too soon to see if there’s any improvement with this drug, so hopefully by Thursday we will have some answers and get back on the right track.
He is still intubated and kind of sedated going on 5 days now. To prepare for extubation this afternoon, they’ve gone down on his fentanyl and ativan so he’s not super sleepy. He was awake and pretty agitated (which would’ve been a good time to remove it), but he got pre-medicated (Tylenol & benadryl) before his Campath so he’s been pretty sleepy again the past few hours. The transplant team came by and looked at him, and they didn’t seem to want to extubate immediately, but the PICU team does. So if he wakes up again tonight they will remove the breathing tube, if he remains sleepy/comfortable they will wait until tomorrow.
They removed his Vascath (the catheter in his IJ/neck) because it was only being used for pheresis and they don’t plan to do anymore of that, so there was no more need for that catheter. They started him on lovenox injections today because of the blood clot in his right arm where his PICC is. They’ll let those work for a few days, do an ultrasound to make sure the injections are treating the clot and then pull that line as well. His blood pressures have been looking good, so they went down on his blood pressure meds today. One of the ICU doctors mentioned pulling his arterial line, which is a catheter placed in an artery and is able to give them blood pressures constantly. But his nurse, bless her for advocating for him, told them to reconsider because yes removing lines is a good thing, but is it really a good idea to start removing it before we’re absolutely ready then risk the chance of having to place another one in a couple days? If theres nothing wrong with it, it just makes sense to leave it, especially while it is still being utilized. So we will see what the final decision is on that in the morning.



That’s all the updates I have for now. Please keep praying & sending all your positive thoughts our way!
Since Jaxsons room number seems to be changing more frequently than we anticipated, it might be easier to start sending cards & packages to the Ronald McDonald House:
Ronald McDonald House
C/O Katherine Dahl #1205
451 44th st
Pittsburgh, PA 15201
You can also send ecards on the hospitals website & they will be printed and delivered to his room:
https://ecards.upmc.com/getwell.asp
The hospital is Children’s hospital of Pittsburgh and his room number is 514.
And if you’d like to donate or share our fundraiser page:
Thank you everyone for your continued support. 💚
It has been awhile since I have updated the blog, and I wish I had some good things to write about but unfortunately things started to go downhill again. Jaxson’s body is still rejecting the organs. He has been on a second anti-rejection med (Thymoglobulin) as well as steroid boluses. Together, both of those meds have a lot of side effects; high blood pressure & high blood sugar being the two that Jaxson had problems with the most. Around 3am on March 6th, his nurse came in to give him his scheduled pain medicine (the previous day he had started complaining of more pain) and she noticed he wasn’t acting quite right. He would respond when someone talked to him, but he wouldn’t look at anyone. I got up to see if I could stimulate him with no luck. The ICU doctors were called in. A few seconds later his oxygen dropped and he started seizing. The whole thing lasted about 5 minutes but it was still a scary experience. He was transferred to the ICU, they did a CT scan, and an EEG. The CT scan showed something called PRES (Posterior reversible encephalopathy syndrome) which was brought on by the high blood pressure from the meds to fight the rejection.

Since he had been on the rejection treatment meds for about a week now with no significant change, they decided to start something called plasmapheresis. This removed his blood, then separated and replaced the plasma. It lasted about 3 hours and was done once a day for three days. The reason for the plasmapheresis was because he had high antibodies. Typically, thats a good thing. Your immune system naturally forms antibodies to fight against infections and viruses. But, they also want to attack transplanted organs because they see it as something foreign. So, they removed his plasma which is where these antibodies were forming, and replaced it with new plasma.
He stayed in the PICU for about a week with no more seizures and his blood pressures seemed to be stabilizing, though he was still in a lot of pain. He was moved back up to the transplant floor on Saturday. Monday morning (today), the doctor came in to look at him before his scope/biopsy and noticed his ileostomy had prolapsed from him crying and being agitated. He had been on narcotic pain meds, which made his breathing slow down more while he slept, so they decided to move him back down to the ICU after his scope. He was sedated for the scope/biopsy and will remain that way until at least tomorrow so they can get his breathing, and blood pressures more stabilized. It will also make him more comfortable pain wise, and less agitated.
We are praying that todays scope/biopsy showed a lot more improvement since the plasmapheresis because we are seriously running out of options on how to treat this rejection. There is one more med they can try but they don’t like to use it unless they absolutely have to. It suppresses the immune system so much and for a long time that he will literally pick up every single virus.
Praying for better tomorrows.
We’ll figure the rest out.
Thank you so much again to everyone who has sent cards, toys, and words of encouragement, we appreciate it so much!

We’ll figure the rest out.
The other day, I was reminded of a previous blog post I had written and I mentioned an article on parenting a premature/medically fragile child. There was a specific quote in that article that I loved, and in this moment it is exactly what I needed to see. I needed that reminder. (Thank you Shawn.) We’ve been in the hospital two weeks now and knowing that we still had months to go, I could feel myself getting more emotional with each day that passed. Which I think is par for the course, I don’t think anyone could go through what we’ve gone through and not break down at least once. So I needed to see this quote and remind myself of it everyday in order to get through this.
It doesn’t matter how frequently we visit the ER or how long he’s admitted, because as long as he lives we’ll figure the rest out.
In a way, this quote has also reminded me to focus more on the positive and less on the negative. I am so happy to be in a hospital that strives for excellence and is dedicated to patient care. Im glad we have a transplant team who are thoroughly educated, and know exactly what they’re doing during every step of this journey. I’m grateful to have an amazing support system back home who make me feel less alone during this journey. I’m incredibly thankful for our anonymous donor family who chose organ donation and gave Jaxson a chance to have a healthy, “normal” life. So even though we are almost 2000 miles away from home, both of us are going stir crazy in this hospital room, and some days are harder than others: As long as he lives, we will figure the rest out.

Jaxsons biopsy & scope on Thursday showed the rejection was severe. The doctors expected this since he had only been on the extra dose of the anti rejection medicine for two days. Since then, he has improved more and more each day. The rejection caused him to be in some pain, but for the last two days he hasn’t needed any pain medicine. Physically he is improving so we can only hope the the scope & biopsy on Monday will show that he’s improving internally as well. Unfortunately, since the rejection he has needed extra doses of steroids too and this caused his blood sugar to increase significantly. So yesterday he was seen by an endocrinologist and she ordered insulin for the time being. Yes, this means he is poked with a needle multiple times a day (hopefully the pokes will lessen each day). But child life here is great and gave his nurse a box of toys, so after each poke Jaxson gets a prize and he soon forgets anything even happened. He’s more willing to get up and play again, and likes to get out of bed and sit on the couch with me. That’s about all I have to update on as the rest is just a waiting game. Thank you everyone who continues to send cards & gifts and just be there for us. Jaxson really loves getting mail everyday. 🙂
💚💚💚
Post transplant day 10
So last night (2/25), Jaxson spiked a fever and seemed to be in more tummy pain than he was earlier. The nurses drew cultures from every line & peripherally, did a urinalysis and swabbed his nose to check for viral infections. They did this to cover all of their bases & find the source of the fever since not many signs led straight to rejection. They started antibiotics immediately and stopped feeds as well. This morning he went down for his ileoscopy and biopsy. The scope looked normal & the stoma appeared swollen but they thought maybe that was just from the extra fluids given last night since the color still looked good. The biopsy results would take a few hours to come back but in the mean time, the urinalysis from last night came back positive for a uti and the nasal swab was positive for two different colds (rhinovirus and enterovirus). The doctor ordered a CT scan, and for that had to place a peripheral IV- which they finally got on the third try. And guess what? Since both the urinalysis and nasal swab came back positive, they figured they found the source(s) of the fever and cancelled it. Three IV pokes for nothing. Around 4:30, the biopsy results came back and showed the intestine was definitely in rejection. This of course is likely the main cause of the fever and tummy pain. The plan is to give him steroids today and tomorrow, as well as a second anti-rejection med tomorrow morning and hopefully that will knock it out. They will do another biopsy Thursday to see where things stand and go from there. His doctors anticipated him rejecting at some point and typically isn’t as bad as it sounds. So I’m praying the intestines will respond well to the extra meds and he can get back on the right track again.

Post transplant Day 6
So, I want to put some peoples minds a little more at ease with some information I’ve been learning over the last couple of days. I also want to mention really quick that while this transplant was needed to improve Jaxsons quality of life- it comes with its own set of potential complications. He will be on anti-rejection meds his whole life. That alone comes with some risks. (Weakened immune system). Like I said, this was desperately needed, but sadly modern medicine isn’t to the point yet where we can put a different organ in our body and have it be 100% okay.
So with that being said- rejection is the number one thing we worry about, though it isn’t as scary as it sounds. If he were to go into rejection, they would increase the dose of his anti rejection meds and maybe add a couple new ones until his body accepts it again. One good thing about transplanting a liver with an intestine is somehow it decreases (but doesn’t eliminate) the chance of rejection. There is also more chance of the intestine rejecting than the liver, but again either can reject at anytime. Just because one organ is in rejection does not mean the others are too. They are able to tell if the liver is rejecting by blood tests, but are not able to see if intestines are rejecting until they do a scope & biopsy. Another thing we worry about post transplant is infections. The anti rejection meds are suppressing his immune system so his body doesn’t fight off (reject) the new organs. The more anti rejection meds he is taking, the lower his immune system is. He will be on these meds his whole life, but the dose will likely decrease the farther out from transplant he gets. We’ve been told he doesn’t have to live in a bubble, but to use common sense. 😊
Jaxson had his first scope and biopsy today and everything went great. I was able to be in the room with him and he didn’t cry once. They put the scope about three inches into his ileostomy, took a couple pictures & did the biopsy and it was over in about five minutes. The doctors got the results back a few hours later and everything looked normal; no signs of rejection. He will have these done two times a week for a few weeks. Tomorrow he will have his upper GI study where they’ll put contrast through his gtube and watch it move through the intestines on an X-ray. If everything looks good he will be able to start having clear liquids- which I know he will be happy about because he misses his water!
And today was another great day. He is getting back to his normal self more and more each day. His pain is pretty well managed, so he was able and willing to walk to the playroom not once, but twice today! He also sat up in his bed a lot more today and played with toys. I’m sorry I don’t have much to update on, but as they say- no news is good news!

I also want to mention that as I’m writing this, it’s 40° and rainy. We sure are missing our Arizona sun! Counting down the days until we can soak it up again.
And I of course want to thank everyone who has reached out, supported, and prayed for us! We couldn’t do this without so many amazing people standing behind us!
💚💚💚
Post transplant update.
Jaxsons Transplant surgery lasted 11 hours and he did incredibly well. He didn’t swell too much from fluids given in the OR, so they were able to fully close his belly. He came back up to the room intubated and sedated and remained that way until Saturday afternoon. They weaned him from the muscle relaxer med so he started to move around and was more alert by about noon. He wanted to pull his breathing tube out, so they put him to room air with just a little help from the ventilator and he did well for about an hour. Around 3pm they pulled the breathing tube and he has done well ever since. His pain has been well controlled as he is getting a small amount of pain medicine continuously through his IV. We have the option to push the button and give him a little more as needed, but he has rarely needed the extra dose. Yesterday, they removed the peripheral IVs that were placed during surgery (which is nice because now his hands and feet are free) and he moved out of the PICU and back up to the transplant floor. He will have an endoscopy done on Thursday to look at the intestines and do a biopsy to make sure there are no signs of rejection. He will have these done once or twice a week for awhile. He has an ileostomy now (similar to a colostomy; but a colostomy brings part of the colon to the abdominal surface and an ileostomy brings the last portion of the small intestine to the abdominal surface).The ileostomy makes it much easier to scope and take biopsy’s as they can just go through that instead of the other way; it should be less invasive. After his scope on Thursday they will do an upper GI study with contrast to make sure everything is moving as it should and after that they will start feeds. If everything keeps going as it is, he can be discharged and to off the Ronald McDonald House with me in a week or two!
If anyone would like to send cards the address is:
Jaxson Dahl c/o 7B #726
4401 penn ave
Pittsburgh, PA 15224
I know he would appreciate having things to open and to show him how much he is loved. 💚

